Cvp and Art Line Set Up and Management Nursing Ceu
The arterial line pressure transducer setup
The arterial line pressure transducer setup
This chapter is vaguely relevant to Section G7(iii) of the 2017 CICM Primary Syllabus, which asks the test candidate to"draw the invasive and non-invasive measurement of claret pressure level, including limitations and potential sources of error". It is also loosely associated with Section G7(2),"depict the principles of measurement, limitations, and potential sources of
mistake for pressure transducers, and their calibration". Information technology represents a summary of the important concepts for the purpose of rapid revision, with a focus on arterial blood pressure measurement.
The demand for such a summary is not clear in the context of the CICM Role I examination, every bit the examiners take only ever interrogated the trainee's understanding of these matters one time, in Question two from the start paper of 2019. "Hydraulic coupling and transducers" formed an of import part of the answer there. Overall, the subject matter seems like something foundational to ICU practice, and in his attempt to explain these bug to himself the author had written all-encompassing notes on the subject field early in his career. It seemed wasteful to destroy them, and they are reproduced here for sentimental reasons every bit much as for educational ones.
In summary, the components of the measurement arrangement and their characteristics are equally follows:
- An intra-arterial catheter
- Kink-resistant, biologically inert, incompressible
- Accesses the arterial apportionment and provides the interface between the arterial blood and the circuit fluid
- Fluid-filled tubing
- Produces the hydraulic coupling between the arterial apportionment and the force per unit area transducer
- Access points to let sampling
- Flush valve
- Fluid in the tubing
- Incompressible
- Normally, normal saline or
- Under pressure from the pressure purse to forbid claret refluxing into the line
- Counterpressure fluid bag
- Pneumatically pressurised to ~ 300mmHg to sufficiently annul systemic arterial pressure
- Pressure transducer
- Wheatstone bridge piezoresistive transducer which converts pressure into a change of electrical current
- Signal conditioning and monitoring software
- Filters the raw betoken from the transducer
- Converts information technology into a human-readable waveform
- Records the data in a storage medium for review
The fluid-filled transducer system used for this is the aforementioned as would be found in whatever other system measuring the force per unit area in whatever other fluid-filled compartment (primal veins, cerebral ventricles). The physics behind this is discussed at great length in the affiliate on "Pressure transducers for haemodynamic measurements" and "Resonance, damping and frequency response". These and other entries nether the heading "Principles of Force per unit area Measurement" represent a redux of this affiliate and add picayune to the learning process, in the same way that a 4-hour director's cutting adds footling to the content of a move film which retains all of its positive qualities when cutting past 50% for movie theater release.
Arterial Line Transducer Setup
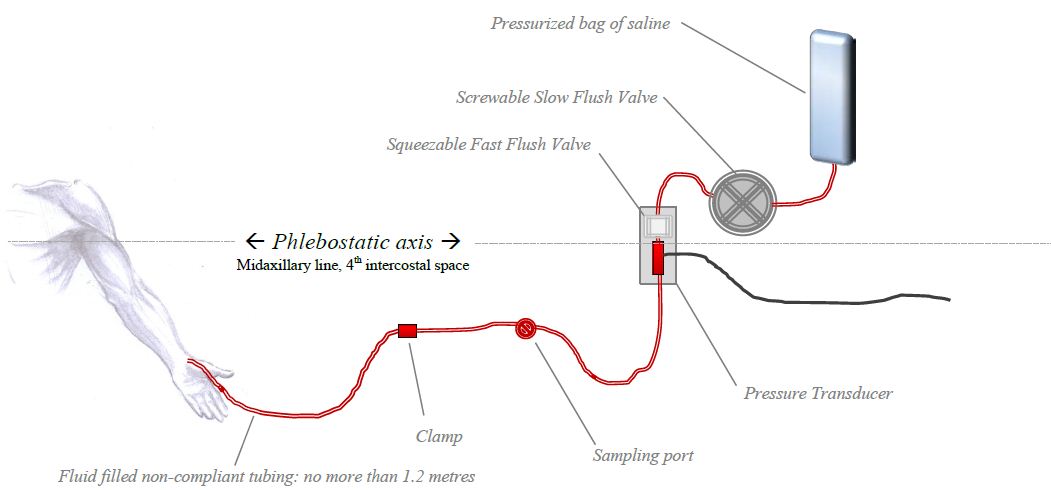
The arterial force per unit area wave travels at 6-ten metres/sec. The cannula in the avenue is continued to the transducer via some non-compliant fluid-filled tubing. The transducer is unremarkably a soft silicone diaphragm attached to a Wheatstone Bridge. It converts the pressure change into a change in electrical resistance of the excursion. This tin can exist viewed as waveform.
Priming the non-compliant pressure level tubing
The thought is that the fluid in the tubing transmits the pressure moving ridge to the transducer - The whole principle rests on a continuous cylinder of saline connecting the artery to the pressure level transducer. The design and engineering characteristics of this tubing has a significant influence on the role of the whole transducer system.
Damping
Without restating the cloth discussed in the chapter on resonance and damping, one can simply say that "damping is anything that has a "daze absorber" consequence on the art line. Air bubbles, long tubing, narrow tubing or soft compliant tubing – all of these absorb some of the force of the pulse wave decreasing the amplitude of the oscillations. This is one of the reasons normal IV tubing is not used to set up an arterial line transducer kit: the IV tubing is also soft and compliant. An excessively rubberband length of tubing will cause damping by absorbing the energy of the pressure moving ridge, wasting information technology on deforming the walls of the transducer set (which will depend on the viscosity of the tubing material). The professional-sounding style to express this concept in the examination would exist to say that elastic tubing increases the damping coefficient. To alter a diagram from Gardner (1981), which describes the relationship between damping coefficient and resonant frequency on art line waveform interpretation:

And then: taking an otherwise adequate arterial line trace and increasing the damping by increasing the elasticity of the tubing will accept information technology into an unuseable overdamped territory. Overdamping results in a slurred waveform with overestimation of the diastolic and underestimation of systolic; however, the MAP value is usually preserved. In contrast, a kinked or clogged art line will encounter MAP systolic and diastolic all trending towards nix.
Resonance
The fluid-filled system has a sure natural frequency of resonance. In an ideal system with some sort of perfectly inelastic tubing, the major determinant of this natural frequency is the length of the tubing: the longer the tubing, the lower the natural frequency. The patient's pulse oscillation is normally a fairly low-frequency phenomenon, and as the tubing length increases, the natural frequency approaches the patient'south pulse wave frequency. The organization so resonates, amplifying the indicate. Thus, the longer the tubing, the more than resonance in the organisation, and consequently the system will be underdamped. For the aforementioned reason, the tube lumen should always exist no smaller than 1.5mm. To use the aforementioned diagram from Gardner:

Then, equally y'all tin can encounter, increasing the length of this ideal inelastic tubing will also pull the transducer set into a territory where information technology loses its clinical utility. Even so, no tubing is "platonic" - it cannot be a rigid burnished piping in society for information technology to remain clinically usable. So: what is the net outcome of increasing tubing length in the existent globe?
Cyberspace effect of tubing length on resonance and damping coefficient:
why only 1.ii meters of tubing?
Aye, length of tubing can increase the resonance, and it tin can besides cause overdamping. The longer the tubing, the lower the natural frequency of the transducer system, so theoretically the more than resonance. On the other hand, an excessively elastic length of tubing will crusade damping by absorbing the energy of the pressure wave. In other words, longer tubing increases the damping coefficient and lowers the natural frequency. To put this on Gardner's diagram:

Zeroing and levelling the fine art line
Zeroing and levelling are occasionally used interchangeably, but they are not the aforementioned thing. They tend to occur together in the clinical setting, but the terms describe unlike processes. Zeroing exposes the transducer to atmospheric pressure level via an open air-fluid interface, and levelling assigns this zero reference point to a specific position on the symbolic fluid-filled column that is the patient's body.
"Zeroing"can be defined as "the utilize of atmospheric force per unit area as a reference standard confronting which all other pressures are measured". The approved higher definition is "a process which confirms that atmospheric pressure results in a zero reading by the measurement system". The device is zeroed when the air-fluid interface is opened to atmospheric pressure level (otherwise it would read diastolic blood pressures of ~ 760mmHg). Atmospheric pressure varies lilliputian between the intensivists' eye level and the supine patients' aortic root level, then strictly speaking the zeroing of an arterial line can take identify with the transducer lying anywhere. Re-zeroing must occasionally accept place as both the transducer and the atmospheric force per unit area will gradually drift abroad from the calibration point.
"Leveling" can be defined every bit "the selection of a position of interest at which the reference standard (zero ) is set". The canonical college definition is "a process which determines the position on the patient you wish to be considered to be your zero." For reasons of convenience this tends to happen at the same time as zeroing the system to atmospheric pressure (which too sets the reference "0 mmHg" standard), but theoretically one could zero the transducer to atmosphere and then swing it wildly all around the room before levelling information technology against a reference point on the frightened patient.
The system is conventionally "levelled" at the phlebostatic axis, which is a reference level nosotros accept used since probably 1945. The phlebostatic axis corresponds roughly with the position of the right atrium and aortic root, and his level has mostly been accepted equally the ideal reference level for measure out the pressure of the blood returning to the eye. Information technology was therefore adopted every bit the reference level for CVP measurement. For arterial pressure measurements, at least since 2001 or so nosotros have too been levelling the arterial lines at the phlebostatic axis. Prior to that, some units levelled their arterial lines at the level of the catheter insertion site. The specific reference point for the arterial transducer is actually the aortic root, but considering it is very close to the right atrium the ii reference levels are substantially the same.
The scientific basis for these reference points is murky, and relates vaguely to the idea that these are also the reference points from which your ain pressure transducers (the atrial and arterial baroreceptors) "measure" the pressure level for the purpose of maintaining cardiovascular homeostasis. This concept, in plow, relates to the idea of in that location beingness a "hydrostatic indifference point" where pressure and vascular wall stress remain stable irrespective of changes in body position, and which appears to be somewhere around the correct atrium. In that location are actually distinct hydrostatic indifference points for the venous and arterial circulation, and the right atrium is probably non where they are in the normal human (that right atrial location was adamant in the 1930s by rotating the bodies of dead animals), but to discuss this here would stand for an unforgivable digression. More particular is bachelor in the affiliate dealing with the physiological responses to changes in posture. For the purposes of day-to-day use, the arterial line should be zeroed at the "phlebostatic centrality", any that is.
For every 10cm beneath the phlebostatic axis, the art line will add 7.4mmHg of pressure level.
1 may sometimes be interested in levelling the arterial line at another point. Substantially, the level at which you zilch the arterial line volition measure the arterial pressure level at that level. Which means that if your patient is in some sort of anarchistic position (eg. sitting commodities upright) you may wish to measure at the level of the tragus instead. An art line levelled at the level of the external auditory meatus volition measure the arterial pressure in the Circle of Willis, which is a representation of cognitive perfusion pressure. Diverse eminent guild guidelines recommend that for the apply of cerebral perfusion force per unit area as a therapeutic target, the reference level should be somewhere around the middle cranial fossa. Whether this matters or not is a field of study of some fence.
Flushing the art line
Apparently, using heparinised saline improves accurateness somehow, simply does not prolong patency.Most centres have abandoned this exercise because of the increased risk of HITS. The normal rate of flow is 3ml/hr, simply to proceed the catheter from clotting. The flush charge per unit of the fast flush is 30-60ml/min, and then in absence of a expert cannula, one tin can infuse the patient with a litre of flush fluid every 15-30 minutes.
References
I humbly thank Vincent Chen (President of AACN, I think) for helping me bring some sort of gild and accuracy to this set of notes. The quality of this resources is enhanced by his contribution.
Gardner, Reed Grand. "Direct claret pressure measurement-dynamic response requirements."Anesthesiology 54.3 (1981): 227-236.
From Bersten and Soni'south" Oh'due south Intensive Care Transmission", sixth Edition; plus McGhee and Bridges Monitoring Arterial Claret Pressure: What You lot May Not Know (Crit Care Nurse April i, 2002 vol. 22 no. 2 60-79 )
Scheer,Perel and Pfeiffer.Complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in amazement and intensive care medicine. Crit Intendance. 2002; 6(3): 199–204.
For those who like hardcore physics, this fantabulous resources will be an enormous source of amusement. It appears to exist a gratuitous online textbook of anaesthesia.
LITFL also link to this comprehensive FRCA self-assessment document:
Abby Jones, Oliver Pratt; PHYSICAL PRINCIPLES OF INTRA-ARTERIAL Blood Pressure level MEASUREMENT - Amazement TUTORIAL OF THE WEEK 137 8TH JUNE 2009
McCanny, Peter, et al. "Haemodynamic monitoring and management." (2013). PACT, ESICM
This FRCA report certificate on arterial pressure monitoring is a goldmine of detailed information.
Lodato RF, Schlichting R: "Arterial pressure monitoring. Arterial catheterization: complications." In Principles and Practise of Intensive Intendance Monitoring. Book Part Three. second edition. Edited by Tobin MJ. New York: McGraw Hill; 1998::733-756.
Winsor, Travis, and George E. Burch. "Phlebostatic Axis and Phlebostatic Level, Reference Levels for Venous Pressure Measurements in Man." Experimental Biology and Medicine 58.two (1945): 165-169.
McCann, Ulysse G., et al. "Invasive arterial bp monitoring in trauma and critical intendance: Outcome of variable transducer level, catheter access, and patient position." CHEST Periodical 120.4 (2001): 1322-1326.
Thomas, Eastward., M. Czosnyka, and P. Hutchinson. "Calculation of cerebral perfusion pressure in the direction of traumatic brain injury: joint position statement by the councils of the Neuroanaesthesia and Disquisitional Intendance Society of Uk and Ireland (NACCS) and the Society of British Neurological Surgeons (SBNS)." British journal of anaesthesia (2015): aev233.
Gondringer, N., and J. D. Cuddeford. "Monitoring in anesthesia: clinical application of monitoring key venous and pulmonary artery pressure (continuing education credit)." AANA periodical 54.1 (1986): 43-56.
Source: https://derangedphysiology.com/main/cicm-primary-exam/required-reading/cardiovascular-system/Chapter%20758/arterial-line-pressure-transducer-setup
0 Response to "Cvp and Art Line Set Up and Management Nursing Ceu"
Post a Comment